AI can now be used to help scientists discover new drugs in a fraction of the time it would take by conventional methods says Nigel.
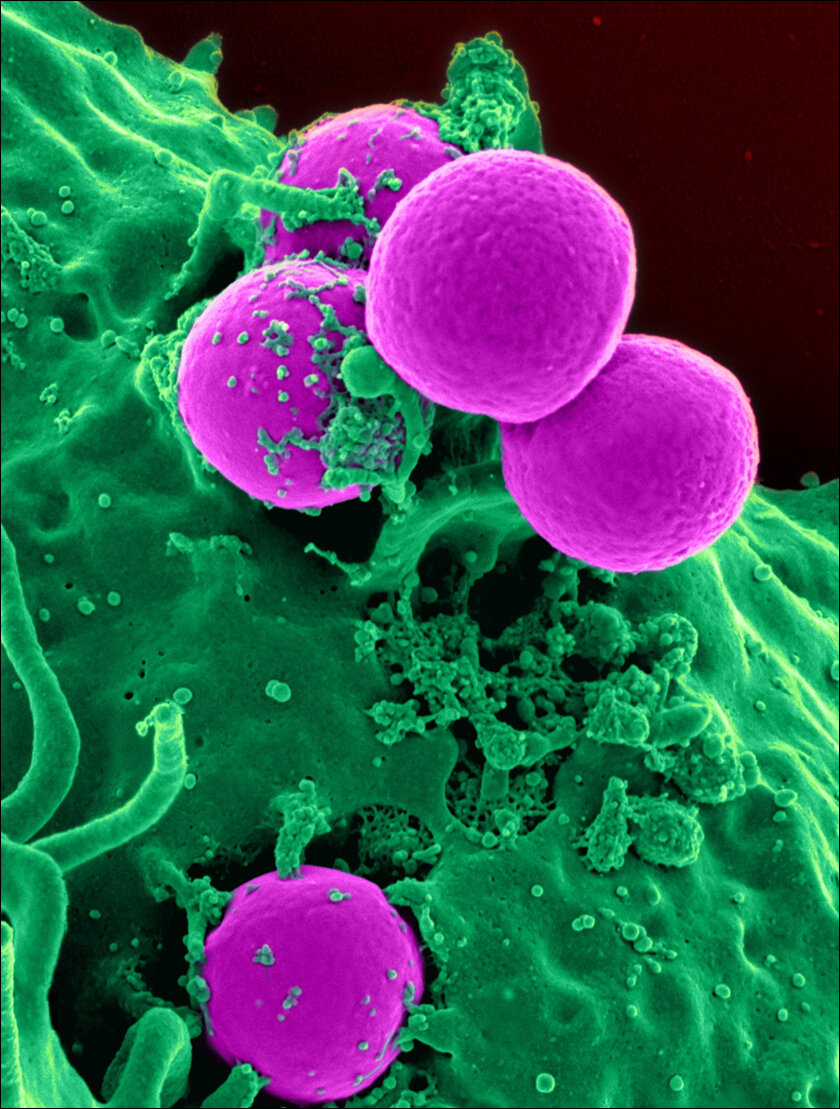
If you have a fear of hospitals in general, you may want to skip this post. Superbugs or Hospital Acquired Infections are very real, and the problem is growing bigger by the day. One in 31 Americans contracts a hospital-acquired nosocomial infection (HAI) each day, according to the CDC (Center for Disease Control). Similarly, according to a recent survey across 120 ICUs in India, HAIs made up 73.3% of blood infections and over 53% of UTI cases.

For the uninitiated, HAIs, also called Superbugs, are pathogens that have grown resistant to the drugs (antibiotics) that are supposed to kill them. That’s right; there are strains of bacteria, fungi, parasites, and viruses that are immune to most antibiotics.
This leaves doctors with very few options for treatment, like the use of alternative antibiotics that are less effective or even older antibiotics which may come with a lot of unhealthy side effects.
Where do Superbugs come from?
The leading cause for the creation of such Superbugs is the misuse of antibiotics, which results in the pathogens developing mutations to fight these antibiotics. These mutations include the development of biofilms to keep antibiotics out, neutralizing agents to break down the antibiotics, reworking their internal structure so the antibiotics don’t work, and efflux pumps to flush the antibiotics out of their cells. Since hospitals are where antibiotics are the most used (and misused), hospitals have become a breeding ground for such disease-resistant strains, adding to people’s fear of hospitals, and rightly so.
Now the biggest problem here is that new antibiotics take decades to be developed, and in the meantime, doctors have to make do with either older or less effective alternatives. All is not lost, however, as scientists are now using neural networks to speed up the process of developing new antibiotics that can fight Superbugs.
According to a recent study in the Journal Nature, a team of researchers from McMasters University and MIT have used AI to discover a new antibiotic that can help heal drug-resistant infections. The study was conducted by introducing 7,500 different compounds to a strain of Acinetobacter baumannii (Superbug) bacteria to see if any of them were harmful to the bacteria in any way.
AI to the rescue
That dataset was then used to train the algorithm to search for similar compounds or compounds with similar properties. Out of a set of 6,680 new compounds, the algorithm successfully isolated hundreds of promising candidates in just a couple of hours. The researchers then chose 240 for further investigation, out of which nine were finally selected as antibiotics. Aubacin, the most effective of the nine, was used to conduct clinical trials on mice infected with the Superbug, the results of which proved its effectiveness in treating wounds infected with Acinetobacter baumannii. What’s interesting is that Aubacin was previously being studied as a drug to combat diabetes, a bit like how Viagra was supposed to be heart medication.
According to the researchers, while Aubacin may not be as effective as modern antibiotics, the fact that Superbugs are resistant to most antibiotics makes it a viable option. Another benefit is that Aubacin only targets Acinetobacter baumannii, and leaves other bacteria, including beneficial bacteria, intact. This ability to zero in on the target is highly desirable since one of the main drawbacks of antibiotics is that it kills beneficial bacteria while also exposing themselves to other bacteria, helping them build resistance. The researchers also noted that Aubacin succeeds where conventional antibiotics fail because it gets in the way of an essential process called lipoprotein trafficking which is basically the process of transporting proteins from inside the cell to the cell wall.

The future of superbugs and antibiotics
A recent study suggests that 40% of people infected with Superbugs at hospital ICUs in India die within 14 days, and this is only the data from the ICUs; the general wards still need to be surveyed. In the United States, Acinetobacter baumanni is the leading cause of infections among troops in Iraq and Afghanistan and is commonly found in hospitals. What makes this Superbug worse is the fact that it can survive for weeks and even months on doorknobs and other surfaces and can lead to pneumonia and even meningitis. Additionally, Acinetobacter baumanni can inherit drug-resistant genes from its environment, making hospitals the perfect habitat to build resistance. The fact that AI can now be used to help scientists discover new drugs in a fraction of the time it would take by conventional methods is a step in the right direction toward making hospitals safe again.
In case you missed:
- AI Uncovers Thousands of Potential Psychedelic Compounds!
- A Glowing Plant Could Be Your New Night Lamp for $29
- Researchers develop solar cells to charge phones through their screens
- From Fridge to Fusion Reactor, How Mayonnaise is Facilitating Nuclear Fusion
- Scientists establish two-way Lucid Dream communication!
- This computer uses human brain cells and runs on Dopamine!
- Could Contact Lenses be the Key to Fully Wearable BCIs?
- Humans Just Achieved Teleportation? Clickbait vs. Facts
- Tiny robots made from human cells can heal wounds!
- What Is Electronic Soil?